
You shouldn’t need to cancel a doctor’s appointment because your ride bailed, or because the only available slot was across town during your work shift. But that’s still the reality for too many people. Healthcare has always been tangled up with logistics — traffic, scheduling gaps, time off work, waiting rooms packed at 8 a.m. on a Tuesday. None of that has anything to do with actual care. It’s just friction.
Telehealth video conferencing removes a chunk of that friction. It cuts out geography. It shrinks long waits into quick connections. You talk to your doctor from the couch, from your lunch break, from wherever you are — and suddenly healthcare starts to feel a little more like service, not a system.
This shift didn’t come out of nowhere. COVID slammed the gas pedal, but the tools were already there — in hospitals, therapy offices, rehab centers. Now, even solo practitioners and small clinics are building their own digital care environments using medical video conferencing as the backbone.
In this article, we’re skipping the fluff and talking about 7 real benefits of telehealth video conferencing — things that actually improve care, boost outcomes, and give both patients and providers more control. Let’s get into it.
Easier Access to Care, Wherever You Are

Let’s be honest — some people don’t skip appointments because they’re careless. They skip because they physically can’t get there. Some don’t drive. Others live two hours from the nearest clinic, and the last bus left yesterday. A 74-year-old with aching knees might look at an icy sidewalk and decide it’s not worth the risk.
Telehealth video conference tools change that. A patient opens their phone, joins a call, and suddenly they’re in the room with their doctor — minus the room. Whether it’s a rural town with no specialists or a city apartment with no elevator, access becomes a screen away.
Take James — 62, diabetic, lives in a village where the local hospital handles everything from fractures to flu. Through video conferencing in healthcare, his check-ins now happen weekly, not quarterly. No long drives. No rescheduling. Just a video call, a glucose log, and face-to-face advice.
And that’s not an edge case. Seniors, single parents, disabled adults — they’re all reclaiming control over their health without having to wrestle with location or transport. Clinics, in turn, see fewer no-shows and more consistent care.
Faster Diagnoses, Fewer Delays

There’s something almost absurd about calling a clinic with a health concern and hearing, “The next available appointment is three weeks out.” It’s not always life-threatening — but it’s rarely acceptable either.
With telehealth video conferencing, that delay often disappears. Need a quick evaluation? You can speak with a nurse practitioner this afternoon. Feeling off after surgery? Your surgeon can check in via video and adjust your meds today — not next Tuesday.
And it’s not just for routine stuff. Take mental health. A psychologist offering same-day video triage can stop a spiral before it deepens. That initial contact, even if brief, can reroute someone from crisis to care.
For doctors, this speed means more than just convenience — it means catching conditions earlier, before they escalate. For patients, it means not having to “wait it out” because there’s no other option.
When a three-minute call replaces a three-week wait, everyone wins.
Increased Patient Comfort & Engagement

A clinic room is sterile. A webcam is familiar. That simple difference can change everything — especially in therapy, pediatrics, and follow-up care. People open up more when they’re not sitting in a room full of fluorescent lights and outdated magazines. It’s not just convenience — it’s comfort. And comfort matters.
Telehealth video conferencing lets people show up as they are, in the places where they actually live. That translates into better conversations and more honest reporting. Doctors aren’t just seeing the patient — they’re seeing how the patient exists in their space. Pets wander by. Kids chime in. Medications are right there on the counter. It’s all useful, human context.
When care happens on your terms, it’s easier to stay engaged. Patients are less likely to miss appointments or drop off after the first visit. Especially in mental health, that continuity is everything.
Here’s what makes a difference:
- No waiting rooms. Just log in and talk.
- No need to explain what “home life” looks like — the provider can see it.
- No pressure to “perform” wellness for a stranger in a lab coat.
For teenagers in therapy, for parents juggling three jobs, for introverts who dread in-person anything — this kind of care feels less like a system, and more like support. And that’s where engagement begins.
Better Collaboration Between Specialists

Medicine has a coordination problem. A cardiologist in one clinic. A general practitioner in another. A radiologist across town. Each writes their own notes. Each guesses at what the others might be thinking. The patient, caught in the middle, becomes the messenger.
Medical video conferencing flips that script.
Now, three doctors can sit in the same virtual room with the patient — not metaphorically, but literally. They can review scans together, share updates instantly, and settle treatment decisions without waiting for faxed reports or callbacks.
This isn’t a luxury for elite hospitals anymore. It’s becoming standard in oncology units, surgical prep, and even chronic illness management.
What Collaboration Looks Like in Practice
| Scenario | Traditional Process | Video Conferencing Alternative |
| Cancer treatment planning | 3 appointments over 2 weeks | One medical video conference session |
| Rehab check-ins with physical & neuro | Alternating weekly visits | Shared triage call with both specialists |
| Medication adjustment for comorbidities | Phone tag between providers | Live conversation with patient & both doctors |
No more delays because one specialist is “out of the loop.” No more missed diagnoses because nobody saw the full picture. When clinicians collaborate in real time, care becomes faster, smarter, and more cohesive.
And for the patient? They feel seen. Not like a chart being passed around, but a person being actively cared for — by a team that’s actually talking.
Cost Savings for Patients and Providers
Healthcare isn’t just expensive because of procedures. The hidden costs add up fast — missed appointments, administrative back-and-forth, hours lost to rescheduling. And that’s just on the provider side.
Patients feel it too. Gas. Parking. Half-days off work just to sit in a waiting room. Sometimes it’s not the appointment itself that’s unaffordable — it’s everything wrapped around it.
With telehealth video conferencing, both sides catch a break. Clinics reduce no-shows dramatically when patients can hop on a call from anywhere. One study showed some providers cutting operating costs by up to 30% just by replacing routine follow-ups with video sessions.
There’s less paper. Less overhead. Fewer rooms to staff. For small practices or overworked hospital units, this isn’t just efficiency — it’s survival.
Patients, meanwhile, gain more than saved gas money. They gain flexibility. No need to cancel because of childcare. No Uber ride across town for a 10-minute consult. It’s easier to say yes to care when the system doesn’t make it hard to show up.
The result? A rare win-win in healthcare: fewer wasted resources, and more patients actually receiving care on time.
Higher Security and HIPAA-Ready Compliance

Medical records are nobody’s business — and that includes the internet’s. When care moves online, privacy isn’t negotiable. It’s a foundation.
That’s why platforms used in telemedicine must meet serious compliance standards: HIPAA in the U.S., PIPEDA/PHIPA in Canada, GDPR across Europe. Not every video app makes the cut — and frankly, many shouldn’t.
But a few do. Google Meet, for example, is used by research hospitals and public health organizations worldwide. It runs securely in the browser, encrypts all communication, and supports HIPAA compliance out of the box. Zoom, with its dedicated healthcare suite, does the same — assuming it’s configured properly.
Of course, that’s only part of the puzzle. For clinics or startups building their own digital health environments, plug-and-play isn’t always enough. You need video tools that integrate with patient portals, scheduling systems, EHRs, or even billing flows.
In telemedicine, trust starts with privacy. And privacy starts with tools that actually respect it.
Fits the Future of Hybrid Healthcare
Telehealth video conferencing isn’t trying to take the place of hospitals or physical clinics. It’s not an either-or situation. What we’re seeing — and what actually works — is a blend. In-person care when it’s needed, remote care when it makes more sense. That’s the future. And honestly, it’s already here.
Hybrid care models have become the norm for thousands of providers. A patient might come in for an initial diagnosis, then handle every follow-up through video. Or maybe they alternate — one visit in person, one at home. It’s flexible, it’s efficient, and it doesn’t compromise care.
Why hybrid works:
- First appointments still allow for physical exams and personal rapport.
- Follow-ups via video reduce time, travel, and scheduling friction.
- Long-term patients get more consistent care without exhausting staff.
Patients aren’t just asking for this — they’re expecting it. And the providers that adapt aren’t just keeping up. They’re creating stronger, more responsive care systems that meet people where they are — both literally and figuratively.
Telehealth won’t replace the doctor’s office. But it might just make it better.
Why Scrile Stream Is a Smart Choice for Telehealth Providers
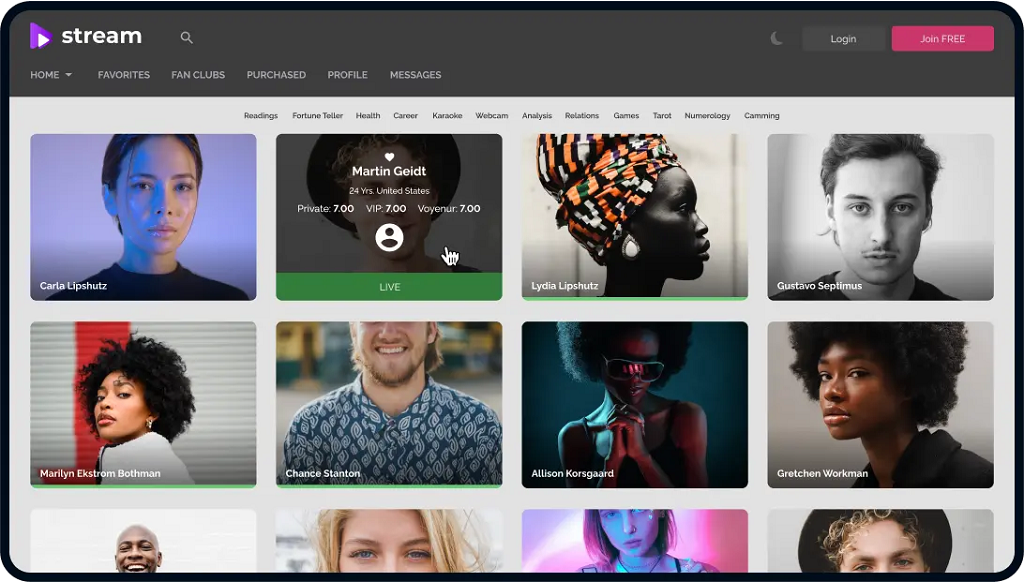
If you’re building your own telehealth infrastructure, most off-the-shelf platforms won’t cut it. You need something that adapts to your workflows — not the other way around. That’s where Scrile Stream comes in.
Unlike generic video conferencing tools, Scrile Stream isn’t a one-size-fits-all solution. It’s a development service that helps you build a secure, branded, and flexible video system tailored to healthcare needs.
Here’s what Scrile Stream enables:
- Secure HD video conferencing with end-to-end encryption
- HIPAA-ready architecture, built with compliance in mind
- Role-based access for doctors, patients, and admins
- Private patient portals with login, scheduling, and notifications
- Built-in monetization tools, including billing and payment integration
- Custom branding and UX, not a white-labeled clone
- Scalable backend, ready for high traffic and multi-location use
Scrile Stream gives you full control — not just over the design, but over the experience. Whether you’re building a digital-first clinic or expanding virtual services, it provides the tools to do it on your terms.
Conclusion
Better access. Less friction. Real connection. Telehealth video conferencing isn’t a cure-all — but it removes barriers that never should’ve existed in the first place.
If you’re ready to build something that actually fits your patients and your practice, Scrile Stream can help. Contact the Scrile team today to start shaping your own telehealth solution.
FAQ
Is Zoom considered a telehealth platform?
Yes — many healthcare providers use Zoom to deliver telehealth video calls for services like mental health, urgent care, and follow-ups. When properly configured, it supports HIPAA and PIPEDA compliance and offers encrypted communication to keep patient data secure.
What is video teleconferencing in healthcare?
It’s a secure, real-time video connection between patients and healthcare professionals. This can be used for consultations, ongoing treatment, or collaborative planning. Healthcare video conferencing helps reduce delays, streamline communication, and expand access to care.
Which video conferencing platforms are HIPAA-compliant?
Google Meet is one example used in hospitals and clinical programs. It runs directly in a browser, encrypts all data, and supports HIPAA compliance without requiring extra downloads or plug-ins.


fantastic post.Never knew this, thankyou for letting me know.